Rapid Response: Workplace Mental Health - Connecting business risk and strategy
The Conference Board of Canada estimates that about 1.3 million Canadian workers suff er from mental health conditions related to anxiety and depression. A significant portion, about 60%, are still at work with reduced hours or capacity, while others are no longer able to work at all. In addition, the Canadian Mental Health Association reports that almost one half (49%) of those suff ering from anxiety or depression have never gone to see a doctor about the problem. This Aon survey asked employers to consider the financial risk exposure presented by employee mental health and the strategies they have in place to address these concerns.
While most organizations support positive workforce mental health through an array of group benefit and in-house support or training programs, a majority (64%) of those polled do not have an organizational mental health strategy that they would consider a key component in their overall people and risk management framework. Organizations are clearly concerned about employee mental health, but the lack of overarching strategy may hamper their ability to design and manage programs that fully address its hard and soft cost eff ects on benefit plans, productivity, and engagement.
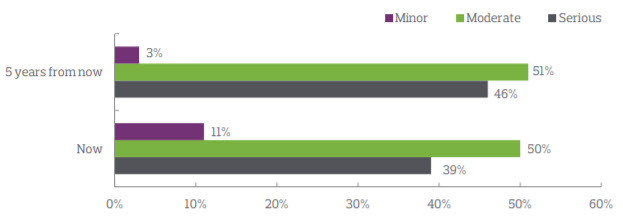
Business risk
Concern about the business risk of mental health is growing and may continue to grow in the future.
What drives mental health strategy?
Employers who have an identifi able organizational mental health strategy are motivated by the desire to reduce costs, support managers dealing with the mental health concerns of their reports, or align with a desired corporate culture, among other things. Among those who don’t, there is concern over cost, and the diffi culty of measuring returnon-investment (ROI) and overall benefi t. The concept of value-oninvestment (VOI) is increasingly replacing the older model of ROI. Financial outcomes are important, but so too is the improvement of employee productivity and engagement.
| Motivating factors |
Rank |
Demotivating factors |
| Reduce paramedical costs |
1 |
Too difficult to measure return on investment |
| Address office conflict, employee complaint patterns, grievances, legal actions, etc |
2 |
Benefits are unclear |
| Satisfy an increased need for manager awareness and training |
3 |
Cost prohibitive resource requirements |
| Align with our desired corporate philosophy/culture |
4 |
Uncertainty about what is involved, or how to begin |
| Reduce drug costs |
5 |
Other organizational priorities at this time |
What are employers doing to support employee mental health?
The vast majority of survey respondents (83% to 98%) identify core benefi t components as supports for mental health strategy. Nearly all provide short- and long-term disability programs, drug benefi ts, employee assistance programs, and paramedical practitioner coverage.
| Non-core efforts to support employee mental health |
|
| Employee assistance program/Employee and family assistance program |
97% |
| Clear and safe process for reporting workplace bullying or harassment |
73% |
| Lunch and learn sessions |
52% |
| Physical health promotion |
52% |
| Personal finance/debt counselling or training |
49% |
| Web-based education programs |
48% |
| Self-help sessions on topics like stress or time management |
38% |
| Health risk assessments |
34% |
| Dietary counselling |
32% |
| Yoga or meditation classes |
27% |
| Prayer space |
26% |
| Telephonic health concierge services |
20% |
| Meditation space |
19% |
| Peer support networks/groups – in person |
15% |
| Technology-based behaviour awareness tools or apps |
13% |
| Peer support networks/groups – online |
1% |
Paramedical coverage
Among the respondents who off er paramedical coverage (e.g. psychology or psychotherapy services), most (63%) have not made recent changes to their plans in reaction to rising concerns over mental health. Public awareness campaigns tell us that several large employers have increased annual caps for psychologist services in a concerted eff ort to help their employees navigate mental health issues. Though efforts like this generate interest in the market, very few of the employers surveyed here (7%) have followed this path to date. Many may be waiting to see whether the early adopters of increased annual caps actually achieve the desired impact of reducing overall benefits costs, and improving productivity and engagement.
It is interesting to note that where psychological or psychotherapeutic service coverage is provided to employee, ninety per cent provide dependent coverage. When considering benefi t design changes, employers should note the impact of dependent coverage, especially in the mental health arena where studies show a rising incidence of mental health issues among youth populations.
Alignment with the national standard
A voluntary standard – National Standard of Canada for Psychological Health and Safety in the Workplace (“the Standard”) – developed by the Mental Health Commission of Canada and its partners, has been in place since 2013. It defines a psychologically healthy and safe workplace as one, “that promotes workers’ psychological well-being and actively works to prevent harm to worker psychological health, including in negligent, reckless, or intentional ways”. The Standard offers a framework upon which to build a psychologically healthy and safe workplace. Only 25% of employers surveyed say they are fully or partially aligned with the Standard. A significant proportion (44%) is unsure of the degree to which their programs align with the standard. The Standard is still fairly new and may be applied with more rigor if concern for the business risk associated with mental health grows, as indicated by the results of this surve.
Among employers with a mental health strategy, what is the nature of its alignment with the National Standard of Canada for Psychological Health and Safety in the Workplace?

Consistent application and measurement
Communication and training are among the greatest mental health program challenges. As an inherently sensitive area to manage, it is vital that policies are applied consistently across organizations and their success and true impact measured and evaluated at regular intervals.
| How is consistent application of policy encouraged? Is policy measured for success/impact? |
Using this method encourage consistent application (%) |
Of those providing this option, what % are actively measuring its success/impact |
| Regular communications with all employees |
54% |
25% |
| Manager training |
43% |
21% |
| New hire training/orientation |
33% |
18% |
| Posters |
20% |
30% |
| Onsite workshops |
27% |
52% |
| Integrated programs (e.g. EAP and disability management) |
24% |
48% |
| Financial support/advocacy from leadership |
15% |
33% |
Acceptance and accommodation
There are a number of approaches to accommodating employees experiencing mental health issues. Depending on the situation, formal accommodation or back-to-work strategies related to a disability may be required. Employers may also utilize options typically associated with formal accommodation practices to alleviate pressure on employees before the situation escalates to disability claim level. The table below sets out current practices as reported by survey respondents.
| Accommodation practices in place |
|
| Flexible hours/scheduling |
59% |
| Flexible location (e.g. working from home) |
47% |
| Reduced hours |
47% |
| We do not have any formal practices in place |
37% |
| Private work areas |
23% |
| Integrated programs |
12% |
| Job-sharing |
12% |
Connecting mental health strategy and business risk
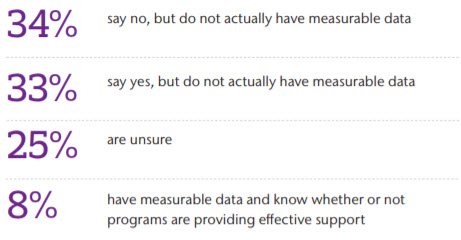
A quarter of organizations are not sure whether their programs are working. Still others think their programs may or may not be having a positive eff ect on their workforce, but they haven’t actually measured the impact. Very few are absolutely confident in their ability to assess their program strategy against specifi c organizational concerns like benefits costs (19%), productivity (9%), or engagement (8%).
Measuring the impact of mental health programs and benefit supports is critical to understanding whether the right programs are in place. Measuring factors like drug and disability costs is a good start. The next step is to establish a line of sight to the relationship between tangible costs and strategic mental health programs. Doing so can lead to core benefit cost savings, and have a positive influence on the less tangible but equally critical costs associated with productivity and engagement.
Do employers feel their current efforts allow them to eff ectively support mental health within their organization?
Methods used to connect mental health strategy and overall business risk
| |
Method |
|
| Review of data in these areas reflects hard costs incurred when a health issue – mental or physical – has progressed to the stage where help has been sought and/or insurance claims have been made. |
EAP/EFAP utilization review |
76% |
| LTD claims incidence review |
71% |
| Overall benefit plan cost review |
70% |
| LTD claims duration review |
68% |
| Drug plan claims review |
68% |
| STD claims incidence review |
64% |
| STD claims duration review |
59% |
| Paramedical benefit utilization review |
55% |
| Review of data in these areas may identify early warning signs for hard costs that may be incurred later |
Formal employee surveys (e.g. via engagement surveys) |
48% |
| Informal employee surveys or feedback |
43% |
| Casual absence data review |
42% |
| Regular internal program audits/reviews |
22% |
| Health risk assessments |
21% |
| Presenteeism assessment |
9% |
* The term “presenteeism” is broadly defined as, “actively at work, but not productive.”
Final thoughts
The results of this survey indicate that mental health is a signifi cant and growing concern for Canadian employers. Addressing mental health is a necessary consideration in the development of a robust organizational people risk strategy. However, uncertainty remains over how to make the strategy work in a cost-effective manner, how to manage it over time, and fi nally how to measure its overall success – both in financial terms and cultural benefit to the organization.