Breaking Down Health and Wellbeing Barriers
To address the workforce health challenges that can lead to poor on-the-job performance, employers are taking an
intentional approach to understanding key barriers to health and wellbeing. There are three targeted strategies that
can help improve affordability and health equity.
1. Aligning Employee Affordability
Employers are improving affordability by focusing on foundational care, including primary care, mental health and
prescription drugs. Nearly half (47 percent) of employers are offering or plan to offer low-cost primary care
services, such as plan design with low copays or waived deductibles. Sixty-two percent are focused on improving
prescription drug affordability, while 65 percent offer or are considering digital tools and self-guided resources
to support emotional wellbeing. Additionally, 35 percent have expanded or are evaluating benefits for employees with
disabilities, such as hearing aids and assistive devices.
These efforts reflect a broader commitment to more cost-effective healthcare benefits.
2. Removing Barriers to Health
Employers are taking meaningful steps to break down systemic barriers to individual health and wellbeing. These
challenges can come in the form of personal circumstances or plan design limitations that make it difficult for
employees and their families to take care of their health.
Employees with caregiving responsibilities often struggle to find time for their own
healthcare needs. Half of employers offer or are considering paid caregiver leave. What’s more, Aon research shows
that 23 percent of employees live in areas with high social determinants of health (SDoH), such as economic
instability, food insecurity and poor access to healthcare services. Nearly half (43 percent) of employers are
offering or considering benefits that address SDoH.
Plan design can also be a barrier to individuals receiving
the care they need. For example, out-of-pocket expenses for cancer diagnostic
services can prevent individuals from following up on cancer screenings that
reveal potential problems. Looking ahead, 40 percent of employers are offering
or considering full coverage for cancer diagnostic services, along with greater
access to screenings, personalized medicine and navigation support.
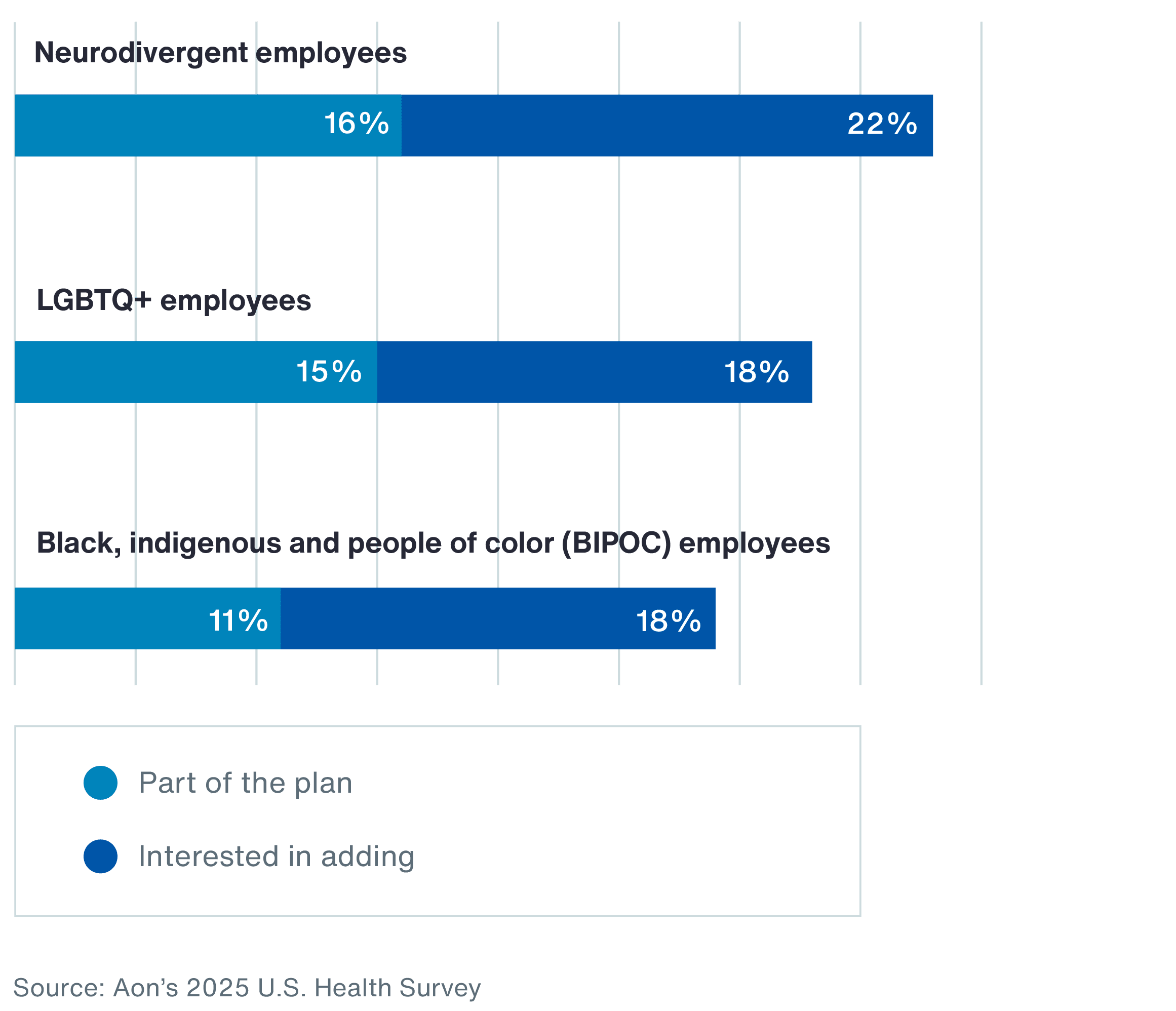
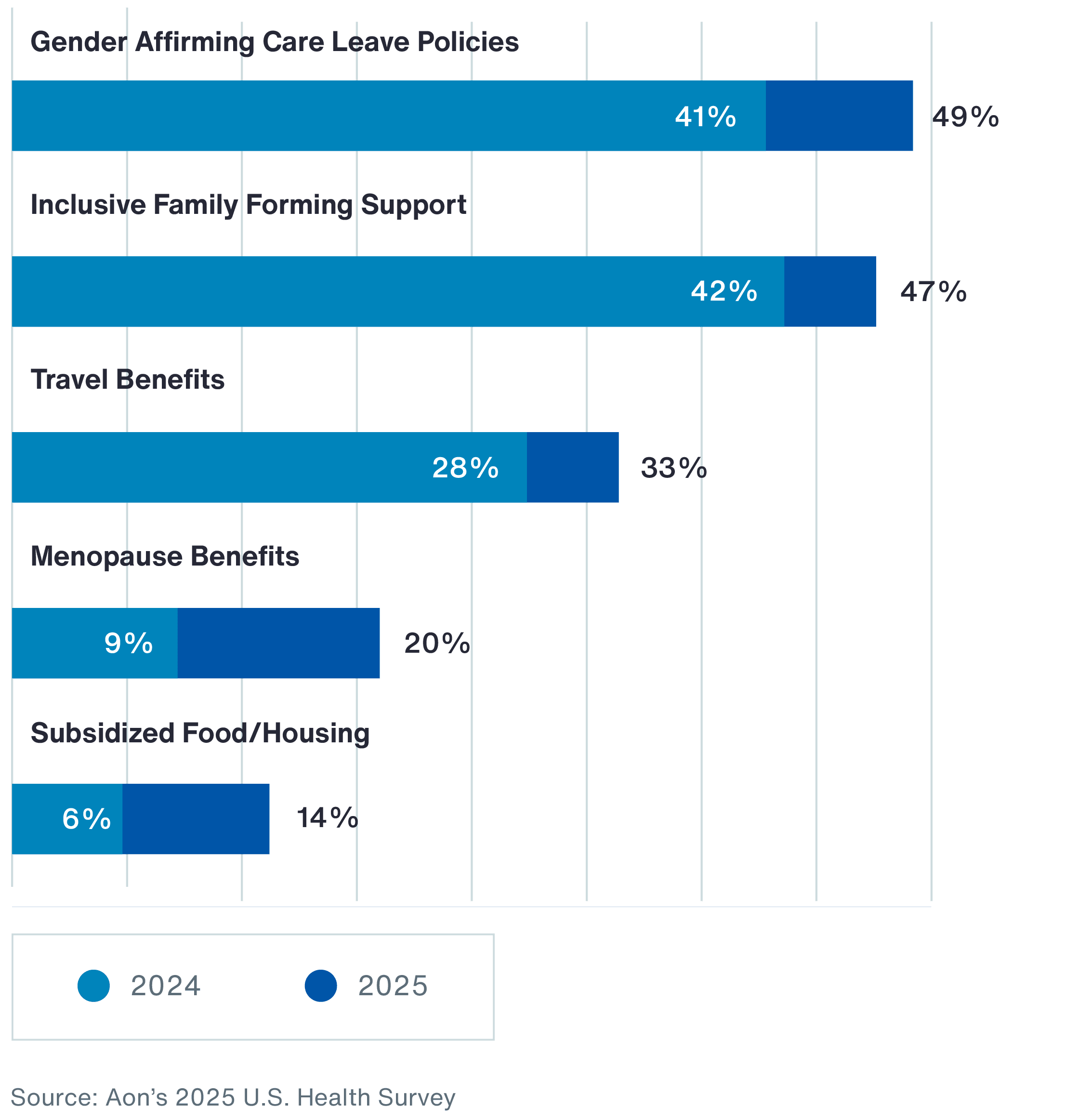
3. Scaling Specialized Care Access
Access to care can be a challenge for individuals with specialized healthcare needs. Many employers are taking action
by offering more inclusive and supportive care to different communities. For example, more employers are expanding
specialized care for neurodivergent, LGBTQ+, and black, indigenous and people of color (BIPOC) populations.
Chart 4: Employers Offering or Considering Specialized Care and Support for the Following Groups